Since Covid-19 began its rampant spread around the world, virus testing has become a highly contentious topic. Issues such as the availability, methodology, cost and reliability of Covid-19 tests are a revolving source of debate and disagreement on social media, within political parties and between international governments. And, assuming an individual receives a reliable positive test result, establishing how healthcare and political systems should manage that patient opens another Pandora’s Box of options – with further compounding conflict.

From April 8, 2020, the Hong Kong government mandated that all arrivals into Hong Kong International Airport submit for Covid-19 testing and 14 days of electronically monitored quarantine and tracking. The test currently involves each passenger producing 5 millilitres of saliva into a vial, which is then transferred to hospital pathology laboratories for analysis using the polymerase chain reaction (PCR) technique. This diagnostic method can identify the presence of the virus from a small sample.
While testing with PCR offers high detection sensitivity when conducted properly, the technique is also delicate and requires excellent scientific method. Because of this, PCR is more likely to yield a false negative result than a false positive in a clinical setting. Negative samples can, however, become cross-contaminated with positive samples if the operator is not fastidious with their technique.

The Covid-19 pandemic exploded with a velocity that outpaced the ability of healthcare systems and medical supply industries to produce the myriad products required to control the spread of the virus, including personal protective equipment (PPE), face masks, respirators and test kits. It, therefore, comes as little surprise that clinics and hospitals around the world have been forced to “mix and match” brands and types of PCR kits, all offering varying levels of sensitivity and accuracy.
These factors have been a cause of confusion and anguish for many, with reports of patients receiving cyclical “positive, negative, positive” results, possibly confounded by the use of PCR testing kits with different sensitivities. In Hong Kong, some Covid-19 patients admitted to public hospitals this year endured stays of up to 60 days.
Additionally, flaws in the Hong Kong government’s hospital isolation protocol must also be playing a significant role in the confusion. Covid-19-positive patients in Hong Kong have been shown sharing wards, toilets, sinks, power outlets, and even taking each other’s temperatures. This nullifies the concept of isolation: something that should be fundamental in a hospital scenario. With every addition into a hospital room, it must be assumed that the 14-day quarantine “day count” reverts to zero, as a strain this contagious can easily cycle through patients.

It is critical that community cases of Covid-19 are identified. Many countries’ economies can only justify testing patients presenting with “cold and flu-like” symptoms. Other countries have no, or limited access to testing kits, relying instead on cumulative symptom-checking to determine a positive case. Alternatively, patients are misdiagnosed after suffering respiratory infections caused by viruses like rhinovirus (RV), respiratory syncytial virus (RSV) and adenoviruses, all of which present in a clinically similar manner to Covid-19.
In Hong Kong, Covid-19 testing is available at government hospitals for around HK$50. However, the virus is so deeply feared and stigmatised that there is little incentive for the general community to be tested. A positive result comes parcelled with potential ramifications: parents being separated from children, the potential trauma of close contacts being sent to a government quarantine facility, admission to hospital for an uncertain period of time, or even the pressure to take a combination of antiviral medications – all outcomes that far outweigh the benefits of testing for many.
A hospital stay is unnecessary for the majority of global Covid-19 cases, with many nations successfully stemming the spread through strictly monitored home quarantines (including severe penalties for any breach), with follow-up testing being sufficient to recover and thrive.

The fears that surround testing in Hong Kong leave mildly ill and asymptomatic individuals intermingling in the community unchecked, spreading the virus widely and silently. The community cases arising at the Kerry Logistics warehouse in Kwai Chung from May 31 highlight other weaknesses within the local system, with one of the patients presenting to local clinics multiple times before being offered a test.
Collectively, all of these situations impact the Global Coronavirus Count and how we believe the pandemic is progressing. The numbers influence how governments and communities make choices about the way forward, our future lifestyles and behaviours. It would be ignorant to accept the relatively low case numbers reported by countries with high population densities, low testing rates and subpar socio-economic, health and hospital systems, such as Indonesia and India. In China, information regarding national testing per capita is not being made available at all.
Throughout the wildfire spread of this pandemic, scientists worldwide have been racing to develop the “next generation” of Covid-19 test kits. The foremost candidate at this point is the rapid antibody blood test, which within minutes (rather than hours or days) can determine if a person has a current infection, or if their immune system has previously been exposed to the virus.
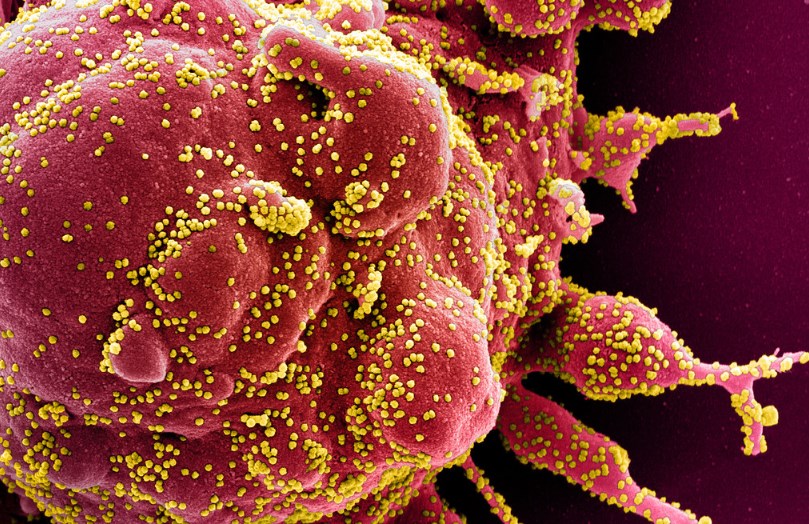
Like PCR testing, antibody testing is confounded with sensitivity and accuracy issues and is also challenged by higher development costs. But, given time, it can become widely available and affordable: over-the-counter and point-of-care-testing antibody tests exist for pregnancy and also diseases like HIV, at a relatively cheap cost to the consumer. If a reliable COVID-19 antibody test could similarly be developed, tested and approved by independent regulatory bodies, this could revolutionise the speed of global social and economic recovery.
On April 15, Emirates became the first airline to conduct on-site rapid Covid-19 tests for passengers, with the results available in 10 minutes. Similar to the “Athlete Biological Passport”, which supports anti-doping in international professional sports, the so-called “immunity passport” may be an option to support safer air travel in the future. However, a universal system must first be developed to accurately corroborate various Covid-19 testing methods and results to be sure that a person’s Covid-19 status could be correctly verified.
Vaccines for other Coronaviridae – SARS and MERS – were never established, and ultimately the outcome may be the same for Covid-19. There are currently hundreds of vaccine candidates in development, and more than a dozen in human clinical trials, all being expedited by enacting every available international emergency regulatory code. But the fact remains that most are only in the first phase of testing, in which safety and tolerability are the key readouts. Putting life on hold for an uncertain period while we wait for a vaccine may be fruitless.
With global financial markets and economies already crippled, the fiscal cost of a fast and reliable test is justifiable when reckoned against the extraordinary cumulative costs of Covid-19 to global healthcare economies thus far. The way forward lies in quickly identifying sick people and carriers, which supports efficient quarantine measures.
Transparent reporting is fundamental, and testing should not be stigmatised. The sooner this takes place, the sooner we can challenge Covid-19, and the world can begin to turn with some degree of normality.
